What's Here? - Table of Contents
Burnout is rising across schools, hospitals, outpatient clinics, and telepractice. The pattern looks the same: good clinicians running out of time, energy, and headspace—not because they care less, but because the work has outgrown the container that holds it. Emotional exhaustion, detachment, and a creeping sense that progress takes too much effort show up long before anyone says “burned out.”
Here’s the truth that changes outcomes fast: burnout is a math problem, not a mindset problem. When load > resources, even elite clinicians struggle. The fix is to rebalance the equation—reducing unnecessary load, increasing real resources, and designing the week so the highest-value work gets protected.
This playbook delivers ten moves that work in the real world. We’ll shift from caseload counting to workload modeling so staffing and schedules reflect minutes, not headcount. We’ll right-size groups, batch evaluations, and use smart templates to cut documentation time in half. We’ll draw clean boundaries that protect mandated minutes and clinical quality. We’ll collaborate strategically—leveraging SLPA support and interprofessional teams within legal/ethical guardrails. We’ll advocate with data (missed minutes, waitlists, travel overhead) so leaders see risk and act. And because sustainability is personal, we’ll put in place energy and recovery protocols that are doable on a Tuesday afternoon, not just during vacations.
What to expect as you move through the guide:
Immediate wins (this week): time-blocking that matches service intensity, documentation snippets, and evaluation batching that frees hours.
Structural upgrades (this term): workload calculators that set realistic caps, service-mix redesign (push-in, consult, tele) that reduces churn, and dashboards that track the metrics that actually matter.
Career durability (this year): role fit, specialty focus, and compensation strategy grounded in market data and cost of living—because the right role in the wrong context still drains capacity.
The outcome we’re driving toward is simple: more services delivered on time, less after-hours paperwork, and a workweek that makes clinical excellence sustainable. Not by “trying harder,” but by deploying better systems.
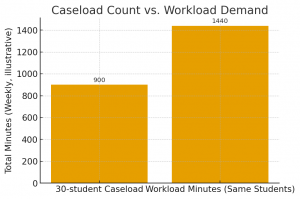
Headcount hides the real problem. Minutes reveal it. Caseload (“30 students”) treats every learner as equal. Workload (“total minutes required to deliver compliant, effective service”) makes capacity visible and actionable.
List service demand by intensity.
Low: 1×20 min/week
Moderate: 1×30 min/week
High: 1×60 min/week
Add consult minutes per student (e.g., 5/10/15) for teacher/caregiver coordination.
Add non-therapy demand.
Evaluations per week × minutes per eval (typ. 120–240+)
Travel/transition overhead (multi-site programs)
Sum total weekly demand minutes.
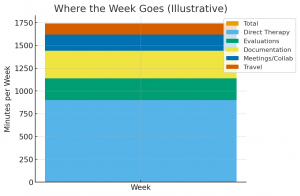
Demand = Direct therapy + Consult + Evaluations + Travel
Define realistic weekly capacity per FTE.
Protect time for documentation and unavoidable admin. As a starting benchmark:
Direct Therapy Capacity: ~1,100 min/FTE/week
Documentation Capacity: ~300 min/FTE/week
Capacity per FTE = Direct + Documentation = ~1,400 min
Compute staffing need and the gap.
FTE needed = Demand ÷ Capacity per FTE
If FTE needed > staffed FTE, the difference is your evidence for redistribution, service redesign, or new hiring.
10 low (20 min) = 200
12 moderate (30 min) = 360
8 high (60 min) = 480
Consult: (10×5) + (12×10) + (8×15) = 290
Evaluations: 3/week × 180 = 540
Travel: 120
Total demand = 200 + 360 + 480 + 290 + 540 + 120 = 1,990 min/week
Capacity per FTE ≈ 1,400 min/week ⇒ FTE needed = 1,990 ÷ 1,400 ≈ 1.42 FTE
With only 1.0 FTE assigned, that’s a 590-minute weekly deficit (~9.8 hours). No amount of “working smarter” closes a math gap this size; the load must be reduced or more capacity added.
Redistribute intensity: Shift 1–2 high-intensity learners or evals to another provider → immediate minute relief.
Service redesign: Convert eligible cases to push-in/consult cycles to maintain outcomes with fewer direct minutes.
Group optimization: Regroup by goal alignment, not homeroom—protects minutes and reduces prep churn.
Fractional capacity: Just 0.4 FTE more (≈560 min) would close the 590-minute gap in the example.
Time protection: Lock 2–3 administrative sprints per week for documentation and eval writing to avoid after-hours spillover.
Rules exist—use them to set defensible limits. Most burnout starts where policy, math, and scheduling drift apart. Bring them back into alignment and caseloads right-size faster than any pep talk.
State/District guidance: maximum caseloads, service-minute requirements, evaluation timelines, make-up minute policies.
Contract/MOU language: workload protections, travel time, documentation allowances.
Program realities: site count, meeting cadence, testing windows.
Convert everything into weekly minutes. Policy without minutes won’t protect capacity.
For each learner: IEP minutes + consult minutes.
Add evaluations/week × minutes/evaluation.
Add travel/transition overhead (multi-site = real minutes).
Sum to a single Demand (minutes/week) figure. Compare to Capacity per FTE from Strategy #1.
This is your objective line between “sustainable” and “overloaded.”
Green: Demand ≤ 95% of capacity (buffer for absences/testing weeks).
Yellow: 96–105% (temporary surge; trigger regrouping or short-term support).
Red: >105% (non-compliant risk; require redistribution, fractional FTE, or service redesign).
Publish these thresholds on the team’s intake sheet so gatekeeping stops being personal and starts being procedural.
Package a one-page brief:
Current Demand vs. Capacity (from the calculator) with the precise FTE gap.
Compliance risk indicators: missed minutes trend, evaluation backlog, time-to-eval median.
Costed options:
Redistribute X high-intensity cases (0 cost; immediate relief).
Add 0.4 FTE (≈560 minutes/week; closes the gap).
Temporary contractor for evaluation blocks during peak months.
Service redesign: increase consult/push-in cycles where appropriate.
Intake guardrail: new assignments require a minutes check—only green/yellow accepted; red triggers the options above.
Escalation: when two consecutive weeks hit yellow/red, leadership selects an option within five business days. Decisions live in writing (reduces back-and-forth and protects service minutes).
Document the FTE gap and projected missed minutes.
Prioritize mandated minutes first; pause non-essential tasks.
Offer a make-up plan tied to added capacity or a defined end date.
This keeps ethics and compliance at the center—and avoids over-promising with inadequate resources.
Time is the treatment plan. When minutes are organized by need and impact—not habit—burnout drops and outcomes climb.
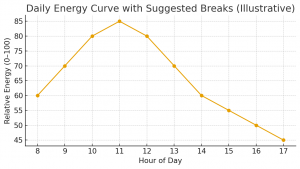
Tier 3 (High): complex AAC, severe language, dysphagia, medically involved cases. Lock these first in protected AM blocks when cognitive energy is highest.
Tier 2 (Moderate): mixed language/phonology, fluency, voice. Place late morning/early afternoon.
Tier 1 (Low): maintenance and consult cycles. Cluster at the end of the day or in brief push-in blocks.
Rule: The higher the intensity, the earlier and more protected the slot.
Goal-aligned grouping: Build around one primary target (e.g., /r/ or syntax) so practice and materials scale.
Size = reps, not chairs: If accuracy <60% or behaviors are demanding, cap at two; otherwise 3–4 is often efficient.
Cycle groups: 6–8-week cycles with planned re-screen → promote or discharge decisively.
Theme days:
Mon/Tue = articulation & phonology
Wed = evaluations + meetings
Thu = language + literacy
Fri = make-ups + consults
Admin sprints: two 45-minute blocks reserved for documentation and phone/email—non-negotiable.
Evaluation block: one half-day/week to test, score, and draft while the data are fresh.
Clinic- or school-initiated cancellations: reschedule within 10 school days; use Fri make-up slots first.
Family-initiated cancellations: document; no auto-make-up unless required by policy.
Storm/testing weeks: invoke “priority grid”—Tier 3 keeps direct minutes; Tier 1 moves to consult/home program.
Does current demand exceed 95% capacity?
Yes: place in consult pending redistribution or added capacity.
No: assign to a goal-matched group with a defined end-date cycle.
Is this Tier 3?
Yes: displace Tier 1 first; log the swap to protect compliance.
Will this case require an eval within 14–21 days?
Yes: schedule inside the weekly evaluation block—not in therapy slots.
Color-code intensity tiers, lock protected blocks, and share a one-page week view with teachers/caregivers.
Use recurring calendar holds for admin sprints and the evaluation block; only leadership can override.
Fewer mid-day context switches, higher treatment fidelity, faster eval throughput, and far less after-hours documentation—because the schedule finally matches the clinical reality.
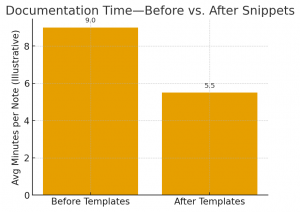
Great therapy needs great notes—just not great amounts of time. Most SLPs bleed hours because documentation is scattered, untemplated, and tackled in tiny fragments between sessions. Fix the structure and the minutes fall fast.
Standardize the skeleton (SOAP/IEP/Progress/Eval).
Batch the work (capture data in-session → write in two sprint blocks per week).
Automate the boilerplate (smart phrases, keyboard macros, voice dictation).
Close the loop with QA (60-second compliance check).
Probe once, write later: quick tally sheets with goal-aligned stimuli; snap a photo or enter counts in a lightweight tracker.
Standard cues shorthand: min/mod/max, visual/verbal/tactile; stop writing paragraphs—use codes.
Group efficiencies: a single probe form listing all students/goals keeps inputs consistent and fast.
Pro tip: When accuracy is <60% or behaviors spike, annotate with a two-word modifier (“low reps,” “high cues”)—enough for clinical sense-making without a novella.
Two protected blocks per week (45 minutes each) beat 14 micro-sessions every time.
Sprint A (mid-week): same-day SOAPs + short progress notes.
Sprint B (Fri): eval writing and progress summaries while testing is fresh.
No context-switching: one document type per sprint.
Pair this with the scheduling upgrades from Strategy #3 (evaluation block + admin sprints) to prevent spillover into evenings.
Smart phrases: preset opening and closing lines for common scenarios (teacher/email contact, home program updates, carryover recommendations).
Keyboard macros: one key sequence expands into cueing ladders, goal language, or safety statements.
Voice dictation: dictate interpretation sections and caregiver summaries in a single pass.
Legal/ethical guardrail: Templates never replace individualized content—use them to speed structure, not to clone findings.
Tables beat prose for probe results (date, target, % accuracy, cue level).
1-page dashboard per student/client: goals, last three data points, next target.
Link once, reference often: in EHR/IEP, cross-reference the dashboard so progress notes pull context automatically.
Compliance check: session length, service minutes delivered/made up, signatures, and required disclosures.
Risk phrases: if recommending reductions or discharge, confirm that the data and stakeholder communications are documented.
Use the KPI dashboard to measure the payoff and keep leadership engaged.
Log documentation minutes per month and time to eval (referral → report).
Share trend lines during staffing conversations to justify protected admin time.
Burnout drops when every minute drives outcomes. The fastest path there: standardize on interventions with strong evidence, then make decisions from simple, consistent probes.
Pick winners: For each target (e.g., /r/, morphosyntax, narrative), lock 1–2 interventions with strong effect sizes and tight dosage windows.
Standardize probes: Same stimuli structure, same scoring, same decision rule (e.g., “promote if ≥80% for 3 consecutive weeks”).
Design for reps: Materials that scale across 2–4 learners, with micro-adaptations (cueing ladders, contrast sets) ready to go.
Columns: date → target → % accuracy → cue level → next step.
Decision row at the bottom: continue | intensify | switch.
Keep it visible during sessions; write less later (pair with Strategy #4 templates).
Front-load success: errorless learning for new targets, brief high-rep sets (90–120 seconds), immediate knowledge of results.
Distributed practice: two shorter, high-rep blocks beat one long, low-rep block.
Generalization on purpose: one built-in carryover task each session (teacher or caregiver).
Boundaries aren’t about being difficult—they’re how mandated minutes, evaluations, and quality survive the week.
Email windows: two daily windows; urgent matters via phone only.
Office hours for consults: one recurring block for teachers/caregivers.
Meeting triage: must-attend vs. async update; reschedule non-urgent invites into admin sprints.
Use clear, respectful language to push back on scope creep, reschedule, or request redistribution.
Invoke the priority grid: Tier 3 direct minutes protected; Tier 1 converts to consult/home program.
Document the swap once; prevent “just this once” from becoming policy.
No single provider can hold every task. Delegation within scope and smart teaming convert overload into sustainable service.
SLPA/paraprofessional support: prep, data capture, carryover tasks, and defined intervention steps as permitted by state rules and supervision standards.
Co-treat with purpose: OT/PT/psych for shared goals (executive function, feeding, AAC), with clear handoffs.
Consult cycles: short, targeted push-in + teacher coaching to reduce direct minutes where appropriate.
Weekly 10-minute huddles with each partner site.
RACI for evaluations and progress cycles (who’s Responsible, Accountable, Consulted, Informed).
Single shared dashboard so everyone sees goals, data, and next steps.
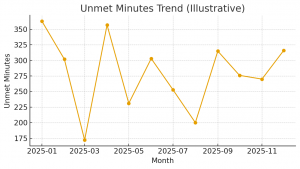
Leaders act when risk and ROI are undeniable. Package both on one page.
Demand vs. Capacity from the workload calculator (FTE gap in minutes and FTE).
Compliance risk: missed minutes trend, evaluation backlog, time-to-eval median.
Options with math: redistribution, fractional FTE, contractor eval blocks, or service-mix shift—each with minute impact and cost.
Plot unmet minutes and time to evaluation; add a dotted line for policy thresholds.
Include a 60-day projection if nothing changes.
Intake enforced at the 95% capacity line.
Two consecutive yellow/red weeks trigger a documented decision within five business days.
All changes logged on the dashboard—transparency reduces friction.
Capacity isn’t just minutes on a calendar—it’s the nervous system behind those minutes. Protect it and the whole caseload runs smoother.
90-second resets between sessions: stand, roll shoulders, 6 slow exhales, one glass of water.
Two movement snacks: 3–5 minutes mid-AM and mid-PM (walk the hallway, light stretch).
One “no-screen” lunch: 15 minutes off email/EHR; eat, breathe, reset vision.
Noise & light hygiene: reduce harsh noise; use softer task lighting to cut fatigue.
Evening guardrails: a 60-minute pre-sleep tech-down window; same wake time daily.
3-minute decompression: jot two bullet takeaways, one next action, then close the chart.
Brief co-regulation (if needed): step outside the therapy room, two slow diaphragmatic breaths, then transition.
Admin sprints stay sacred (from Strategy #3): no meetings dropped on top.
Friday “close loops” ritual: sign the week’s notes, confirm next week’s top three priorities.
Monthly calibration: glance at KPIs—time to eval, documentation minutes, cancellations—and adjust the schedule before small problems stack up.
The most sustainable career is the one that fits the work and the life. When role, setting, pay, and geography align, burnout drops because the system finally supports the clinician behind the schedule.
Which tasks drain the fastest (travel, eval volume, behavior intensity, documentation load)?
Which wins energize the week (AAC breakthroughs, group language, dysphagia, voice)?
Use this map to target roles that amplify energizers and shrink the drains.
Schools → Outpatient/Tele to reduce travel and testing-week chaos.
Acute → Outpatient for more predictable hours and follow-through.
Secondary → Elementary for different behavioral/academic demands.
Hybrid/Tele days to consolidate documentation and consults.
Nominal pay: median wages by occupation.
Real pay: adjust for cost of living so decisions aren’t fooled by big numbers in expensive regions.
Prioritize roles and locations where real pay and workload balance intersect.
Large, diverse markets increase role options, supervision depth, and ladder steps.
Use Top States and Top Metros employment charts to prioritize places with more teams and roles to grow into.
Tie every ask to minutes and outcomes:
Workload cap aligned to the calculator’s FTE math.
Protected admin sprints and a weekly evaluation block.
Service-mix redesign (push-in/consult cycles) where appropriate.
PD budget tied to the specialty you’re building (AAC, voice, dysphagia, literacy, fluency).
Pick one specialty for the next 6–12 months; ship real outcomes and collect artifacts (dashboards, protocols, case studies).
Mentor or precept once capacity is green—you’ll multiply impact and create succession leverage.